Reducing excessive glycolytic activity in early diabetes
An early sign of islet failure is the loss of normal patterns of pulsatile insulin release. Pulsatility is important to normal insulin regulation of hepatic glucose production. Pulsatile insulin also delivery reduces blood glucose more effectively than continuous delivery. Patients with T2D and their close relatives show disruptions in pulsatile insulin secretion.
At the islet level, we reported that mouse islets that were incapable of pulsatility in 11mM glucose (i.e. post-prandial) had reduced capacity for glucose-stimulated insulin release compared to pulsatile islets (Jahanshahi et al., Endocrinology, 2009). We recently reported that a left shift in glucose sensing in islets from diabetic db/db mice is linked to disruptions in pulsatility in 11mM glucose (Corbin & Waters et al., 2016), due at least in part to elevated glucokinase activity. This left shift in glucose sensing can cause excessive insulin release in low glucose (relative hyperinsulinemia) and beta-cell exhaustion that results in inadequate insulin release at post-prandial glucose levels.
As shown in the accompanying figure, mildly reducing excessive glycolytic rates in diabetic islets with the glucokinase inhibitor D-mannoheptulose (MH) can restore normal pulsatility. MH thus reduces excessive insulin secretion in low glucose and provides periods of rest between insulin pulses, which may improve islet health and downstream insulin signaling. Our central hypothesis is that reducing islet glycolytic activity will improve islet function and delay or prevent the development of T2D.
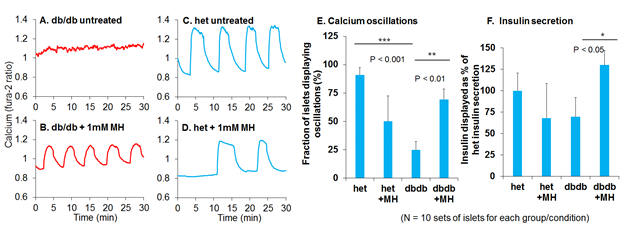
Loss of pulsatility is a hallmark of islet dysfunction in T2D. Disrupted patterns of calcium in diabetic islets (A) can be restored by treating islets with a glucokinase inhibitor (MH) to reduce excessive rates of glycolysis (B). MH treatment thus promotes pulsatility and enhances insulin output from diabetic islets. In contrast, reducing glycolysis in normal islets has mild inhibitory effects (C-F).
Our current work is focused on:
- Determining if glycolytic pulsatility is required for normal islet health and function.
- Examining how shifts in islet glucose sensitivity impact pulsatility, insulin secretion, and insulin signaling.
- Reducing islet glucokinase activity to delay or prevent the onset of hyperglycemia in db/db mice.